Let’s face it: we have all been in the situation where you get some blood work done by your doctor and all you get is ”everything looks ok, all within the reference ranges”. But usually, that’s it. No additional lifestyle advice, no comments on the specific results, and all you got was a conclusion that you are not acutely sick.
I wanna share with you a concrete example of why getting just a typical ”all within the reference ranges” answer isn’t often enough. For example, you might have borderline diabetes, developing insulin resistance, and a chance to develop metabolic syndrome.
Enter glucose.
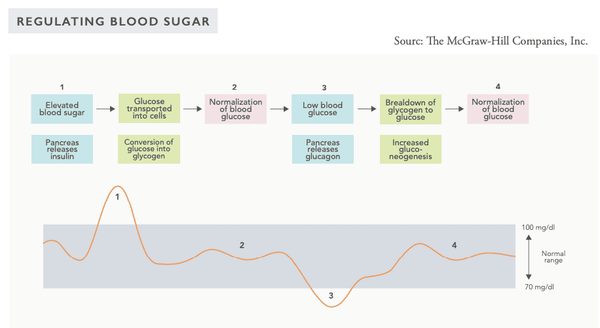
The body's blood sugar regulation mechanism is a very sophisticated system that is affected by several hormones secreted by internal organs. The blood sugar level is regulated by a so-called negative feedback system – this system seeks to bring the body into a state of systemic homeostasis, i.e., a stable equilibrium.
When the blood sugar level is high, pulsations of hormones such as insulin are secreted into the circulation, lowering the blood sugar level. Conversely, when the blood sugar level is low, glucagon and other hormones are secreted into the circulation to increase the blood sugar level.
The systemic blood sugar level monitoring takes place in the beta-cells of the islets of Langerhans in the pancreas as well as the glucose-sensing neurons of the hypothalamus in the brain.
Sleep deprivation has a significant impact on blood sugar regulation. Being significantly sleep-deprived (four hours of sleep per night) for as little as a week impairs the use of glucose for energy and raises fasting blood sugar. It is also a predisposing factor for sugar metabolism disorders (pre-diabetes). According to a study, individuals who sleep less than 6.5 hours per night have up to 40 % lower insulin sensitivity compared to those who get a normal amount (7–8 hours) of sleep per night. Impaired insulin sensitivity is a predisposing factor for blood sugar swings, obesity and type 2 diabetes.
WHICH MARKERS ARE NEEDED FOR TOTAL GLUCOSE HOMEOSTASIS?
FASTING BLOOD SUGAR (FPG)
Glucose is the primary cellular energy source. The glucose levels in the plasma reflect the glucose intake from food, the breakdown of liver and muscle glycogen and the glucose produced via gluconeogenesis. High levels of fasting glucose may be caused by insulin resistance, severe acute stress or certain illnesses. Glucocorticoid drugs also raise the glucose level. Low levels of fasting glucose occur after fasting for several days or in association with certain medical conditions or excessive insulin doses.
– Reference range: 4–6 mmol/L
– Optimal: 4.0–5.3 mmol/L
– Recommended by the Life Extension Foundation: 4.0–4.7 mmol/L
GLYCATED HEMOGLOBIN A1C (HBA1C)
The hemoglobin in red blood cells is glycated by the glucose present in the blood. Glycated hemoglobin levels represent the average blood sugar levels within the preceding 2–3 months. If the glucose levels have been elevated during this time period, the hemoglobin A1C test will also produce higher than normal results. This is indicative of blood sugar dysregulation, insulin resistance or diabetes.
HbA1C values may also be affected by individual factors, particularly with nutrition, which may skew the results somewhat. A study found the lifespan of red blood cells in diabetics to be only 81 days whereas for non-diabetics it was 146 days. The longer the lifespan of the red blood cell, the more it binds glucose (becomes glycated). This may raise the values disproportionately without indicating insulin resistance or pre-diabetes. This may be relevant in cases where the fasting blood sugar and fasting insulin levels are optimal yet the HbA1C level is surprisingly high.
– Normal: 20–42 mmol/L / 4.0%–6.0%
– Optimal: 20–34 mmol/L / 4.0%–5.3%
FASTING INSULIN
Insulin is a hormone produced and secreted by the beta-cells in the pancreas. The body secretes insulin as a response to elevated blood glucose levels that are caused by eating or the secretion of cortisol due to increased stress. Insulin increases glucose absorption and storage and the synthesis of fatty acids and proteins while inhibiting the breakdown of proteins and fatty acids.
Insulin inhibits lipolysis or the breakdown of fat into energy. If the body's stored insulin levels are consistently elevated, the fatty acids circulating in the blood are stored in the adipose tissue. This is called lipogenesis. In particular, the secretion of insulin is stimulated by high blood sugar levels and a carbohydrate-rich diet. Abundant protein intake also increases insulin secretion. Due to these factors, the fasting insulin level should be quite low, in the lower half of the reference range. High insulin levels may also be a predisposing factor for the chronic diseases discussed in the description of the HbA1C value.
Reference range: 2.0–20 mIU/L
HOMA-IR (INSULIN SENSITIVITY)
Homeostatic model assessment (HOMA) is a method of assessing the beta cell function of the pancreas and insulin resistance (IR) from the fasting blood sugar and insulin levels. HOMA has become a widely and globally used clinical and epidemiological tool. The calibrated normal value in HOMA is one (1).
By calculating the interaction between fasting glucose and fasting insulin, the beta-cell function of the pancreas and the insulin sensitivity of the body may be assessed. Insulin sensitivity depends on how much insulin needs to be secreted to store a certain amount of glucose. Insulin sensitivity is present when only a small amount of insulin is needed to store a certain amount of glucose in cells. Conversely, insulin resistance is present when more insulin is required to store an equivalent amount of glucose.
But let’s get a little deeper into the lifestyle factors affect blood glucose homeostasis…
Lifestyle choices that improve insulin sensitivity include:
- Getting sufficient sleep
- Regular exercise (particularly strength training and high-intensity training)
– Combining aerobic exercise and strength training is the most effective way to improve insulin sensitivity - Stress management and reducing stress
- Weight loss (particularly around the waistline)
- Plentiful intake of soluble fibers from food
- Eating more colorful vegetables, berries and fruits (particularly dark berries such as blueberries and blackcurrants)
- Using herbs and spices in cooking
- Reducing the intake of carbohydrates, particularly sugars
- Regular fasting and intermittent fasting
- Avoiding excessive sitting
- Eliminating processed vegetable oils and trans fats from the diet
- Certain dietary supplements may improve insulin sensitivity (covered in detail in the course!)
As you can see from above, the regulation of glucose metabolism is pretty complex, and measuring just your blood glucose levels will not reveal your body’s overall glucose homeostasis.
Do you want to know better what is going on within your body? Come and join us in this unique online learning course! The offer is valid for only a couple of days. And there is simply no risk, we have a 30-day money-back guarantee.
For your health, Dr. Olli Sovijärvi, M.D.





